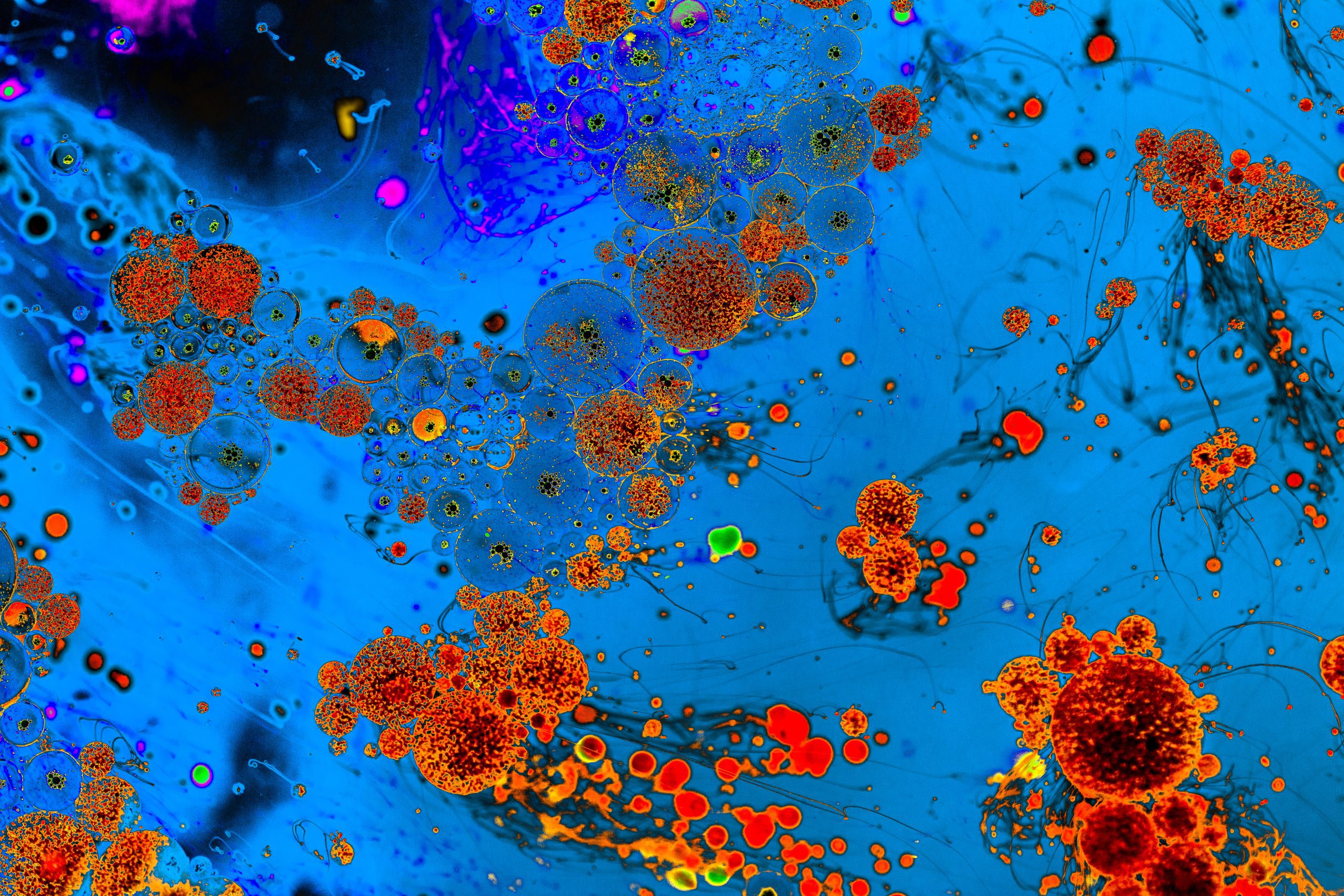
Microbiome Products
Forging a path for your microbiome product
Navigating the complexities of development, approval, and commercialization
KEY FIGURES
50+
Microbiome programs supported
20+
Live biotherapeutic products (LBP)
30%
Advanced to clinical stage

Pioneering Innovation in the Microbiome Field
- Leading the advancement of the microbiome regulatory framework, working with regulators, associations and expert groups
- Award-winning microbiome team (2023 TOPRA for communication)
Comprehensive Product Expertise
Proven experience and a wide range of expertise to guide development of ingredients, of live/inactivated micro-organisms alone/in consortia, and of substances derived from microbiome as drugs (including LBPs, ATMPs), tissue- and cell-based products, medical devices, IVD/CDx, nutraceuticals, and cosmetics.

FAQs
What regulatory framework should be followed during the international development of a microbiome product?
The relevant regulatory framework should be defined on a case-by-case basis, taking into account, in particular, the region(s) of interest and the characteristics of the microbiome product.
Regulations and, therefore, product positioning may vary from one region to another. Standards and/or guidelines specific to the type of microbiome product of interest may be used, as well as non-product specific, transversal references.
Their technical formats are significantly different. While the IND is published to the FDA in the eCTD format, a clinical trial application (CTA) in the EU under the CTR must be processed through the online platform called the Clinical Trials Information System (CTIS). This format mostly relies on data/information entered into the system’s forms, as well as a number of documents, generally in PDF format.
For example, for live biotherapeutic products (LBPs), both the US and the EU have set requirements specific to this type of product. Principles established in local and international guidelines for biological products can be followed, such as the ones from the EMA guideline on quality documentation for biological investigational medicinal products in clinical trials and from the ICH guidelines on the quality of biotechnological products. Finally, transversal materials can also be (partially) applied, such as the FDA Guidance for Industry: INDs for Phase 2 and Phase 3 Studies: Chemistry, Manufacturing, and Controls Information and the ICH General Principles for Planning and Design of Multi-Regional Clinical Trials.
read more
Under what conditions can microorganisms be incorporated in medical devices (MD) ?
To qualify as an MD in the EU, the product should not include viable microorganisms that achieve or support the intended purpose. These must also be considered in determining the risk class of the MD.
It should be demonstrated that the microorganisms incorporated in the MD have no potential for metabolism or multiplication.
Appropriate validation should be put in place to demonstrate the absence of viable microorganisms in the final product.
read more
RELATED GLOSSARY

Questions? Get the answers by our expert team
No two product development paths are the same. Talk to our experts about your development challenges and we will provide you actionable recommendations.
